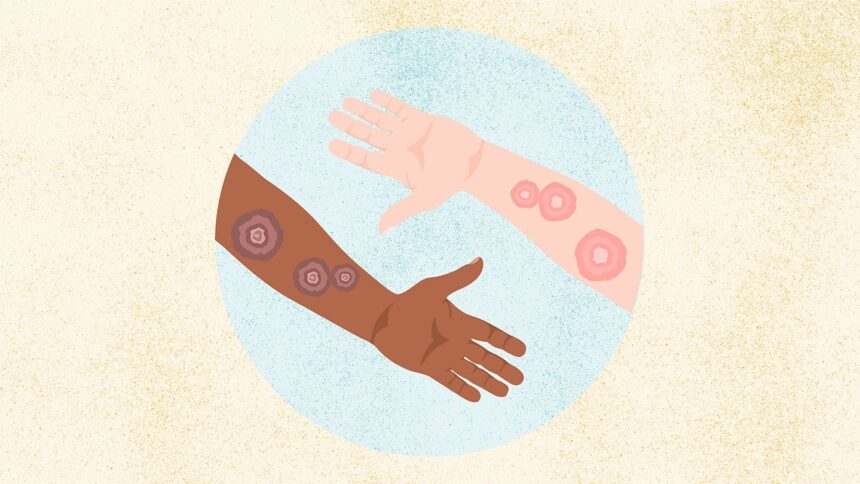
Ringworm (*dermatophytosis*, or tinea infections) is actually one of the most common fungal skin conditions you’ll encounter – despite its misleading name! (1) The nickname “ringworm” comes from the telltale signs: an itchy, red, ring-shaped rash. According to the Centers for Disease Control and Prevention (CDC), this characteristic appearance helps define it.
It’s important to clarify that *nothing* about ringworm involves actual worms; it’s purely a fungal infection caused by dermatophytes – mold-like fungi found in the *Trichophyton*, *Microsporum*, or *Epidermophyton* genera. (1) These infections manifest differently depending on their location, but they all involve contagious fungal spores thriving in warm, moist environments.
Here are some common types based on affected areas:
* **Tinea Pedis**: Known colloquially as athlete’s foot, this type typically appears between the toes.
* **Tinea Cruris**: Commonly referred to as jock itch, it affects the groin, inner thighs, and buttocks.
* **Tinea Barbae**: This is beard ringworm, occurring mainly in facial hair areas for men.
* **Tinea Faciei**: Affects the face.
* **Tinea Manuum**: Occurs on the hands.
* **Tinea Capitis**: Scalp ringworm, which is more frequent in children than adults. (2)
* **Onychomycosis** (*Tinea Unguium*): Nails are affected by this form of fungal infection.
Symptoms vary slightly with location but often include itchy skin, redness, scaling, and sometimes cracking or blistering:
* Athlete’s foot: Peeling, swelling, itching between toes (especially pinky), redness on soles/heels; severe cases may have blisters.
* Jock itch: Itchy, scaly, red spots usually found in the groin crease or inner thighs.
* Beard ringworm: Scaly, itchy red spots on cheeks, chin, and upper neck; can crust over, fill with pus, and cause hair loss there.
* Scalp ringworm: Typically presents as a distinct, scaly, red, circular bald spot that’s itchy. (2)
Ringworm is contagious even before symptoms appear! (4) It spreads through direct skin-to-skin contact with an infected person or animal – including common carriers like cats and dogs, especially kittens and puppies – playing in areas contaminated by fungi, or sharing items used by someone with the infection.
**Diagnosis:**
A healthcare provider can often identify ringworm visually due to its characteristic appearance. However, because it sometimes resembles other conditions (like eczema on the body), a definitive diagnosis may involve microscopic examination of skin scrapings or a fungal culture sent to a lab. The American Academy of Family Physicians notes that distinguishing tinea from similar-looking dermatitis is crucial.
The good news? Most cases respond well to treatment, typically clearing up within two weeks for topical infections and one to three months for scalp ringworm requiring prescription medication. (10) Preventive measures are vital during diagnosis to avoid spreading it further.
**Treatment & Prevention:**
While some mild forms like athlete’s foot or jock itch can be managed with over-the-counter antifungal creams, powders, or solutions containing active ingredients such as clotrimazole, miconazole, terbinafine, and ketoconazole, scalp ringworm usually requires prescription treatment (like griseofulvin, terbinafine, itraconazole, or fluconazole) lasting one to three months. Treatment duration also depends on the specific type.
Alongside medication, simple lifestyle changes can significantly improve symptoms and speed up recovery:
* Wear loose-fitting clothing.
* Avoid tight shoes that cause chafing if you suspect athlete’s foot.
* Shower promptly after exercise or sports activities.
* Keep skin clean and dry, especially in warm climates where sweating occurs frequently.
Prevention is key! To lower your risk of getting ringworm or passing it on:
* Refrain from sharing personal items like clothing, towels, combs, razors, or shoes/socks with others. (5)
* Practice good hygiene: wash hands regularly and bathe thoroughly.
* Avoid contact with infected animals unless they’ve been treated by a vet; ensure pets are checked periodically.
**Complications:**
Usually, ringworm remains relatively confined to the outer skin layers. However, without treatment or if it affects people with compromised immune systems (like those living with HIV/AIDS), it can occasionally invade deeper tissues – leading to a more persistent condition called *Majocchi’s granuloma*. This presents as raised bumps and pustules that are harder to treat.
**Research & Statistics:**
Fungal skin infections, including ringworm-related ones, affect an estimated 10-20% of the global population. (17) While some types are more common in children – tinea capitis being a prime example – Johns Hopkins Medicine notes that overall, fungal infections remain widespread worldwide.
**Related Conditions & Causes:**
Ringworm often mimics other skin conditions like eczema (*atopic dermatitis*), which is another common cause of itchy, red rashes. (19) Eczema can sometimes be confused with ringworm due to overlapping symptoms, but knowing the difference between these related conditions helps ensure appropriate treatment.
**Complications:**
Untreated ringworm isn’t typically life-threatening, especially for those with healthy immune systems. However, ignoring it can allow the infection to worsen or spread:
* Deep skin infections (Majocchi’s granuloma) are rare but possible.
* Fungal nail infections (*tinea unguium*) require specific treatment and carry a higher risk of recurrence if not fully eradicated. (4)
**Q & A
The Takeaway:**
Ringworm is indeed common, but its manageable nature makes it less daunting than its name suggests. By understanding the different types, recognizing symptoms early, seeking appropriate care, and practicing simple prevention habits like handwashing and avoiding shared items, you can effectively manage and reduce your chances of contracting or spreading this widespread fungal infection.
**Research & Statistics:**
An estimated 10 to 20 percent of the world’s population is affected by tinea infections annually. (17) Some types have distinct age demographics: scalp and body ringworm are most common in children under ten, while jock itch, athlete’s foot, and nail infections peak later in life.
**Resources We Value:**
Our information draws from reputable sources like the Mayo Clinic, Cleveland Clinic, CDC, and the American Academy of Dermatology to ensure accuracy.


![Raw Peach and Raspberry Tart with Mascarpone [Vegan] – One Green Planet](https://top-100-recipes.com/wp-content/uploads/2025/08/Peach-and-Strawberry-tart-150x150.jpg)
![Swedish Rhubarb Crumble [Vegan] – One Green Planet](https://top-100-recipes.com/wp-content/uploads/2025/08/RhubarbPie2_EmmaBjorkman-150x150.png)




